PAIN BASICS
MANAGEMENT OF CHRONIC PAIN
Key points
- The modern management of chronic pain favours a practical biopsychosocial approach, which considers neurobiology and psychosocial risk factors and encompasses a wide range of pharmacological and non-pharmacological treatment options, rather than a biomedical approach purely focused on pathophysiology.1
- There is a need for good communication within an multidisciplinary team to best address patient needs and manage their pain effectively.2
- Due to the multi-mechanistic nature of chronic pain, a multimodal treatment plan combining therapies with different modes of action can improve patient outcomes.3
According to the UK’s National Institute for Health and Care Excellence (NICE), the focus of treatment for chronic pain should be to reduce a person’s pain with the objective of improving their quality of life.4 Pain treatment can follow a multimodal approach using both pharmacological and non-pharmacological agents in a dynamic fashion and taking into consideration the following:5
- Intensity of the pain
- Pathophysiology of the pain
- Complexity of the symptoms
- Presence of comorbidity
- Social context
- Time of the illness
References
- Clauw DJ et al. Postgrad Med. 2019;131(3):185–98.
- Varrassi G et al. Curr Med Res Opin. 2010;26:1231–45.
- Pergolizzi J et al. Curr Med Res Opin. 2013;29(9):1127–35.
- National Institute for Health and Care Excellence (NICE). Key therapeutic topic [KTT21] Medicines optimisation in chronic pain. Updated September 2019. Available at: https://www.nice.org.uk/advice/ktt21. Accessed June 2020.
- Cuomo A et al. J Pain Res. 2019;12:711–14.
Implementing a practical biopsychosocial approach
A practical biopsychosocial approach may be utilised to manage chronic pain, which encompasses a wide range of pharmacological and non-pharmacological therapies, in addition to teaching self-management techniques and psychological/rehabilitative support.1 Adopting such a model may lead to a more multimodal and multidisciplinary approach to chronic pain management, incorporating a range of treatment strategies that are aimed at reducing pain, minimising disability and improving patient quality of life.1
Reference
- Clauw DJ et al. Postgrad Med. 2019;131(3):185–98.
Multimodal therapy
Pain is often multi-mechanistic and therefore its management requires a multimodal approach where combinations of pharmacological treatments with different mechanisms of actions as well as non-pharmacological approaches are used to provide analgesia.1 This is particularly apparent in cases where both nociceptive and neuropathic components are at play, which respond differently to different types of analgesics or therapies (including non-pharmacological strategies such as physiotherapy, psychotherapy and rehabilitation techniques).1
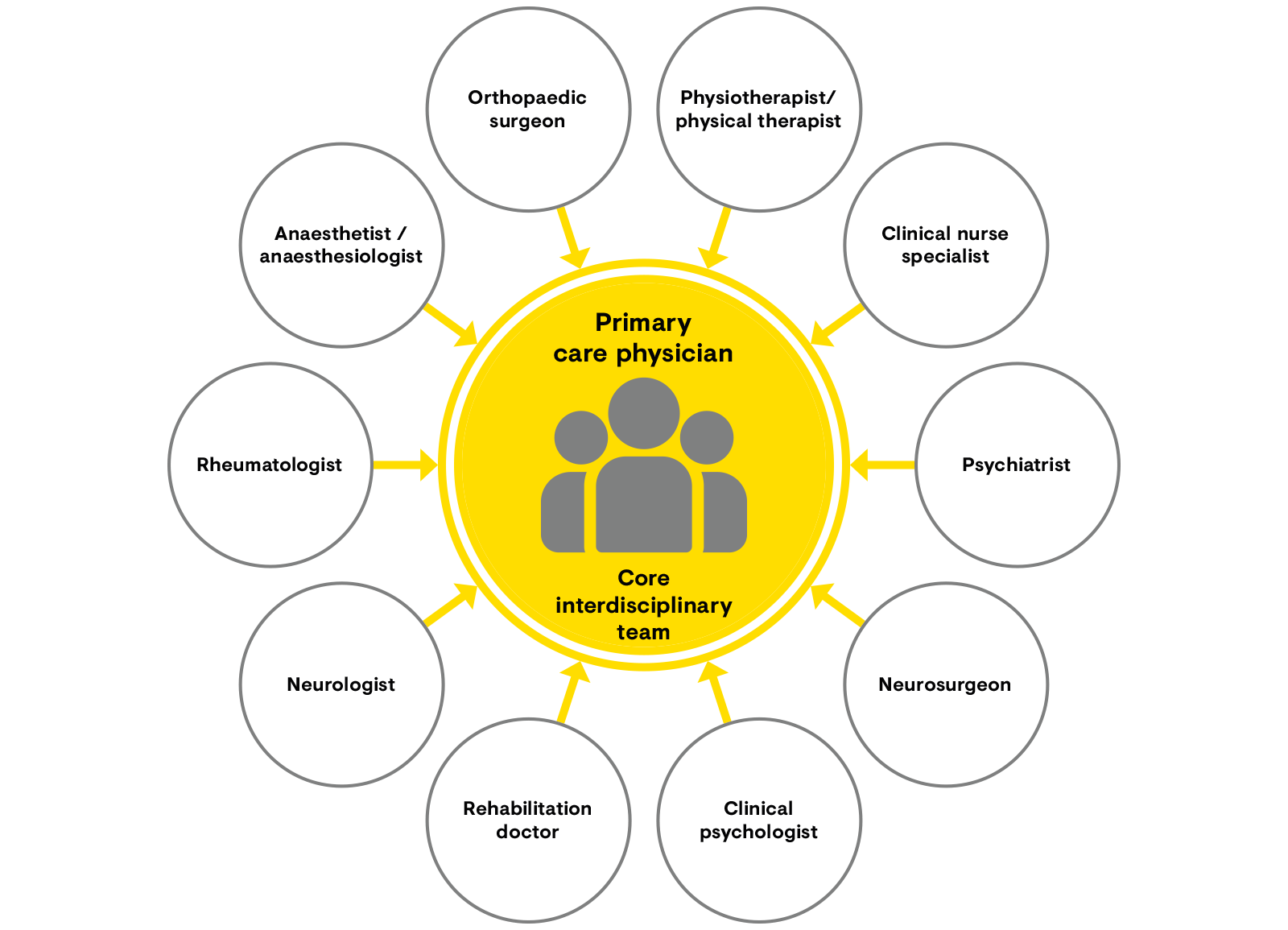
Multidisciplinary management of chronic pain requires a core multidisciplinary team of healthcare professionals.2 The primary care physician acts as gatekeeper and coordinator and has a central role in the long-term management strategy and refers the patient for further treatment as necessary.2 Communication among the team, and between the team and the primary care physician, is extremely important. The multidisciplinary team usually includes a primary care physician, anaesthesiologist, rheumatologist, neurologist and a psychiatrist or psychologist (Figure 1).2 Nevertheless, other specialists may also be included based on the individual patient’s needs. In order to improve outcomes for patients, multimodal therapy delivered by an multidisciplinary team should be considered.
Figure 1: The core multidisciplinary team for the management of chronic pain2
[Adapted from Pergolizzi et al. 2013.2]
References
- Varrassi G et al. Curr Med Res Opin. 2010;26:1231–45.
- Pergolizzi J et al. Curr Med Res Opin. 2013;29(9):1127–35.